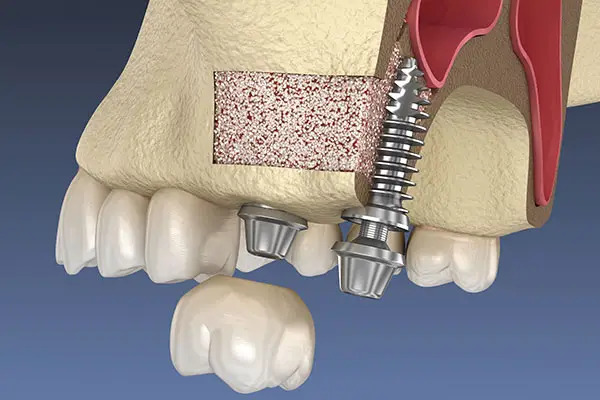
Guided Bone Regeneration (GBR) is a surgical technique employed in dentistry to facilitate the regeneration of bone in areas where it has been lost, particularly in preparation for dental implants. This method involves the use of barrier membranes to prevent the invasion of soft tissue into the bone defect area, thereby allowing for the selective growth of bone cells. The primary goal of GBR is to create a space that is conducive to bone healing and regeneration, which is critical for successful implant placement and the long-term stability of dental restorations [1,2].
The importance of mastering GBR techniques for dentists cannot be overstated. As the demand for dental implants continues to rise, the need for effective bone augmentation strategies becomes increasingly critical. GBR has been shown to yield high success rates comparable to sites without augmentation, making it a reliable option for clinicians [2,3]. Furthermore, advancements in materials and techniques, such as the use of platelet-rich fibrin (PRF) and various types of membranes, have enhanced the efficacy of GBR procedures [4-6]. For instance, studies indicate that the use of PRF can significantly improve bone regeneration outcomes by promoting angiogenesis and osteogenesis, which are vital for the healing process [7,8].
Moreover, the application of GBR is not limited to dental implants alone; it is also utilized in the treatment of various periodontal defects and conditions such as peri-implantitis [9,10]. The versatility of GBR techniques allows dentists to address a wide range of clinical scenarios, thereby expanding their treatment capabilities. For example, the use of bioresorbable membranes has been shown to reduce complications associated with traditional collagen membranes, such as inflammation and immunogenic responses [11]. This adaptability in treatment approaches underscores the necessity for dentists to be proficient in GBR techniques.
In addition to technical skills, understanding the biological principles underlying GBR is crucial for successful outcomes. The interaction between the barrier membranes, growth factors, and the host’s biological response plays a significant role in the healing process [12]. For instance, the incorporation of mesenchymal stem cells and growth factors into GBR protocols has been shown to enhance bone formation and improve overall treatment success [8,12,13]. Thus, a comprehensive understanding of these biological mechanisms will enable dentists to optimize their GBR strategies and achieve better clinical results.
In conclusion, GBR is an essential technique in modern dentistry that facilitates bone regeneration and supports successful implant placement. Dentists should master GBR not only to meet the increasing demand for dental implants but also to enhance their clinical practice by providing effective solutions for various bone-related challenges. The integration of advanced materials and a solid understanding of biological principles will further empower dentists to achieve optimal outcomes in their GBR procedures.
References
- Alauddin, M.S.; Hayei, N.A.A.; Sabarudin, M.A.; Mat-Baharin, N.H. Barrier Membrane in Regenerative Therapy: A Narrative Review. Membranes 2022, 12, 444, doi:10.3390/membranes12050444.
- Tal, H.; Moses, O.; Nemcovsky, C.E. Bioresorbable Collagen Membranes for Guided Bone Regeneration. 2012, 10.5772/34667, doi:10.5772/34667.
- Cardoso, A.C.; Idalgo, F.A.; Sílvio Antônio dos Santos, P.; Nunes, A.G.; Kassis, E.N.; Cicareli, Á.J. Major Aspects of Mesenchymal Stem Cell Signaling and Differentiation Into Osteoblasts in the Optimization of Bone Formation for Dental Implant: A Systematic Review. Mednext Journal of Medical and Health Sciences 2023, 4, doi:10.54448/mdnt23207.
- Alauddin, M.S.; Ramli, H. Management of Membrane Exposure Utilizing Concentrated Growth Factor (CFG) in Guided Bone Regeneration: A Clinical Report. The Open Dentistry Journal 2020, 14, 763-768, doi:10.2174/1874210602014010763.
- Cortese, A.; Pantaleo, G.; Amato, M.; Howard, C.M.; Pedicini, L.; Claudio, P.P. Platelet-Rich Fibrin (PRF) in Implants Dentistry in Combination With New Bone Regenerative Flapless Technique: Evolution of the Technique and Final Results. Open Medicine 2017, 12, 24-32, doi:10.1515/med-2017-0005.
- Lei, L.; Yu, Y.; Han, J.; Danhui, S.; Sun, W.; Zhang, D.; Chen, L. Quantification of Growth Factors in Advanced Platelet‐rich Fibrin and Concentrated Growth Factors and Their Clinical Efficacy as Adjunctive to the GTR Procedure in Periodontal Intrabony Defects. Journal of Periodontology 2019, 91, 462-472, doi:10.1002/jper.19-0290.
- Soni, R.; Priya, A.; Yadav, H.; Mishra, N.; Kumar, L. Bone Augmentation With Sticky Bone and Platelet-Rich Fibrin by Ridge-Split Technique and Nasal Floor Engagement for Immediate Loading of Dental Implant After Extracting Impacted Canine. National Journal of Maxillofacial Surgery 2019, 10, 98, doi:10.4103/njms.njms_37_18.
- Tomasello, L.; Mauceri, R.; Coppola, A.; Pitrone, M.; Pizzo, G.; Campisi, G.; Pizzolanti, G.; Giordano, C. Mesenchymal Stem Cells Derived From Inflamed Dental Pulpal and Gingival Tissue: A Potential Application for Bone Formation. Stem Cell Research & Therapy 2017, 8, doi:10.1186/s13287-017-0633-z.
- Higuchi, J.; Fortunato, G.; Woźniak, B.; Chodara, A.; Domaschke, S.; Męczyńska-Wielgosz, S.; Kruszewski, M.; Dommann, A.; Łojkowski, W. Polymer Membranes Sonocoated and Electrosprayed With Nano-Hydroxyapatite for Periodontal Tissues Regeneration. Nanomaterials 2019, 9, 1625, doi:10.3390/nano9111625.
- Schmidt, E.C.; Papadimitriou, D.E.; Caton, J.G. Surgical Management of Peri‐Implantitis: A Clinical Case Report. Clinical Advances in Periodontics 2014, 4, 31-37, doi:10.1902/cap.2012.120060.
- Quirino, L.C.; Pedro Henrique de Azambuja, C.; Neto, R.T.A.; Comachio, C.A.; Monteiro, N.G.; Ervolino-Silva, A.C.; Okamoto, R.; Pereira-Filho, V.A. Polydioxanone Membrane Compared With Collagen Membrane for Bone Regeneration. Polymers 2023, 15, 868, doi:10.3390/polym15040868.
- Utar, B.; Sunal, G.; Pulat, G.O.; Karaman, O. Human Mesenchymal Stem Cells Osteogenic Differentiation on Dental Barrier Membrane. Journal of Intelligent Systems With Applications 2022, 10.54856/jiswa.202205206, 55-58, doi:10.54856/jiswa.202205206.
- Lim, J.W.; Jang, K.J.; Son, H.; Park, S.; Kim, J.E.; Kim, H.B.; Seonwoo, H.; Choung, Y.H.; Lee, M.C.; Chung, J.H. Aligned Nanofiber-Guided Bone Regeneration Barrier Incorporated With Equine Bone-Derived Hydroxyapatite for Alveolar Bone Regeneration. Polymers 2020, 13, 60, doi:10.3390/polym13010060.